Part of treating your migraine attacks is learning what causes them. Red wine, strenuous exercise, loud noises, stress, and chemical odors can all be migraine triggers for different people.
Seasonal allergies can trigger attacks too. In fact, one study found that 34% of migraine sufferers also had seasonal allergies, and that patients with allergies were over 14 times more likely to get migraine headaches too.
If you suffer from both, you probably have a lot of questions. Do seasonal allergies cause migraine? How can you treat both? How can I tell if my migraine is related to allergies? Untangling it all can be, well, headache-inducing.
In this article, we’re breaking down what we know about how allergies and migraine are related, and what you can do to get some relief.
Allergies 101: What are allergies?
First off, let’s talk about allergies. You’re probably familiar with some of the common symptoms, like a runny nose, sneezing, and itchy eyes. But what exactly happens to your body when you get allergies?
According to Cove Medical Director and migraine expert Dr. Sara Crystal, “An allergy is a hypersensitive reaction to a substance that would not cause symptoms in the majority of people.”
Just like migraine attacks, allergies have triggers. Seasonal allergies, also known as “hay fever,” are triggered by pollen in the air, often in spring and fall. Perennial allergies are similar, except they occur year-round. They are triggered by other things in the air, like mold, pet dander, or dust mites.
Doctors have a term for both seasonal allergies and perennial allergies: allergic rhinitis.
What are the symptoms?
Allergic rhinitis can cause a whole host of unpleasant symptoms, including:
- coughing
- dark undereye circles
- itchy eyes, skin, nose, mouth, or throat
- headache
- hives
- popping ears
- runny or stuffy nose
- sinus pressure
- sneezing
- sore throat
- watery, red, or puffy eyes
Do allergies trigger migraine attacks?
In short, yes, allergies can trigger migraine attacks.
A study found that migraine is more common in people with seasonal allergies, and, if you’re a migraine sufferer, getting seasonal allergies can make your migraine attacks more frequent.
“This may be related to inflammation caused by allergic rhinitis,” says Dr. Crystal, “or by direct activation of the trigeminal nerve from nasal congestion.”
Sometimes allergies cause migraine attacks in a more roundabout way. For example, allergies can interrupt sleep, which in turn triggers an attack. And, according to the American Migraine Foundation, medications used to treat allergies and asthma, like Albuterol inhalers, can also trigger headaches.
Since allergies and migraine can interact in several different ways (even food allergies can cause attacks), it can get a little confusing.
“It’s important to note that migraine and allergic rhinitis are both highly prevalent diseases, frequently co-exist, and may share common mechanisms,” says Dr. Crystal. “People with migraine may experience more severe migraine symptoms with co-existing allergies.”
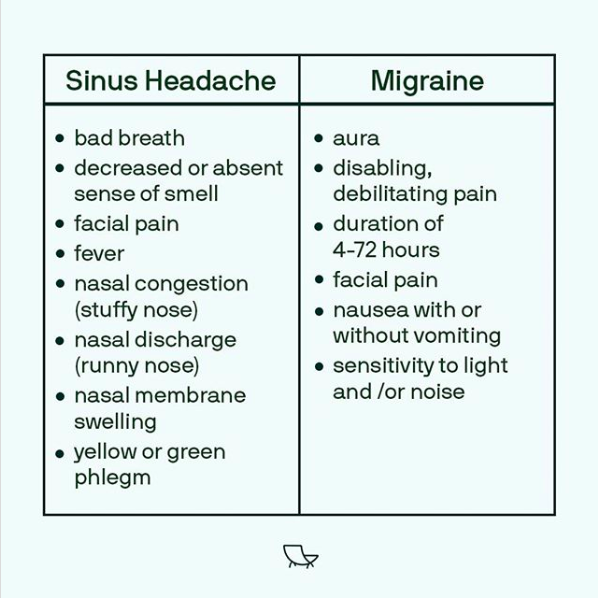
How do you know the difference between a migraine headache and a sinus headache?
Since there is some overlap between migraine symptoms and allergy symptoms, it can be tough to get a diagnosis and find the right treatment.
Dr. Crystal points out, “Both can present similar symptoms—pain over the forehead and maxillary area (around the cheekbones), and autonomic symptoms, such as eye tearing and nasal congestion.”
If you have watery eyes, a stuffy nose, and a bad headache, it might be easy to assume that you’re dealing with allergies and a sinus headache—but it could actually be a migraine attack.
It’s common to mistake the headache that comes along with your allergies as a sinus headache, Dr. Crystal says.
One study found that the majority of patients who had self-diagnosed with sinus headaches actually had migraine. In another study, 88% of patients who thought they had sinus headaches were dealing with migraine.
That said, sinus headaches are actually rare, and there are some obvious differences between sinus headaches and migraine.
Sinus headaches bring on distinctive symptoms you’re unlikely to get with allergies or migraine, such as bad breath, fever, or discolored nasal discharge. They also tend to be caused by an infection, not something that crops up every time your allergies flare.
In addition, migraine headache pain is usually “unilateral and throbbing,” whereas a headache due simply to allergic rhinitis might be “dull and pressure-like,” says Dr. Crystal.
With that in mind, if you have a severe headache along with allergy symptoms, it’s likely you are dealing with allergy-related migraine.
Can treating my allergies prevent migraine attacks?
So, if you have allergies and migraine, what can you do to feel better?
Well, you can start by treating your allergies. Just like with other migraine triggers, avoiding the trigger in the first place can help you have fewer attacks.
One study found that immunotherapy for allergies (i.e., getting allergy shots) helped younger patients get headaches less often.
That said, Dr. Crystal has noticed in her own practice that for some of her patients, starting allergy shots can cause migraine to get worse in the short-term. “Pre-treating with an anti-inflammatory prior to the shots may help.”
Are there medcications that treat allergies and migraine at the same time?
If you have allergies and migraine, it’s a good idea to see a doctor for both. Your primary care physician may recommend you speak to specialists like an allergist or ENT, or a neurologist.
There are plenty of over-the-counter treatments for allergies, including decongestants, corticosteroid nose sprays, and antihistamines. And your doctor may offer other treatments, such as allergy shots or other prescription drugs.
On top of controlling your allergies with medications, your doctor may still recommend you take preventive or acute medications for migraine.
To make it easier for your doctor to diagnose and help you find the right treatment, it’s important to keep careful track of migraine symptoms and possible allergy triggers, says Dr. Crystal.
What about home remedies?
According to a Medline Plus article, some home remedies for allergic rhinitis could help you too, like a nasal wash treatment for manually rinsing your sinuses.
In addition, a Healthline article suggests other home remedies that could reduce symptoms, such as bromelain and honey. As with any home remedies, you should check with your doctor before giving them a try.
Beyond the above suggestions, making lifestyle changes can be a great way to control your allergies. Besides avoiding the things you’re allergic to as much as possible, “allergy-proofing” your home can help.
There’s a lot you can do to allergy proof, like installing a HEPA filter, getting mattress and pillow covers, swapping carpets for hard floors, and keeping pets out of your bedroom (you can get dozens more ideas for allergy proofing from this Mayo Clinic article).
Dealing with migraine pain is tough, especially if you also have seasonal allergies. But, the good news is that both conditions are manageable with lifestyle changes and treatments. The first step to feeling better? Talking to your doctor about your symptoms to see where it makes sense for you to start.
The information provided in this article is not a substitute for professional medical advice, diagnosis, or treatment. You should not rely upon the content provided in this article for specific medical advice. If you have any questions or concerns, please talk to your doctor.
Photo by Louis Hansel on Unsplash


