You’re headed into work when you feel the pain over your cheeks and in your forehead. The head pain quickly goes from dull to throbbing and you're now questioning how you'll be able to sit at a desk all day. You're also wondering how to actually treat it. After all, if it's a migraine headache, you’ll need to take your migraine pain relief medication right away.
But if it’s a true sinus headache, you’ll need to get out your warm compresses and start thinking about whether or not you’ll need a doctor appointment (more on that below). Either way, it's a severe headache and it's the last thing you want to be dealing with right now.
If this scenario sounds familiar, you wouldn’t be the first person to get a migraine headache and a sinus headache confused. The two types of headaches have a lot in common.
Cove medical advisor, Philip Bain likes to bring up a landmark study called the American Migraine Study II.
This study concluded many people who thought that they had sinusitus (a.k.a. sinus infection) were actually diagnosed with migraine. When patients thought that their headache was sinus-related, the overwhelming majority had migraine. Interestingly, in that same study, when primary care physicians thought that they had sinus headaches, again the majority had migraine. This emphasizes just how common it is for migraine attacks to be misdiagnosed as sinus headaches, even by doctors.
What do sinus headaches and migraine headaches have in common?
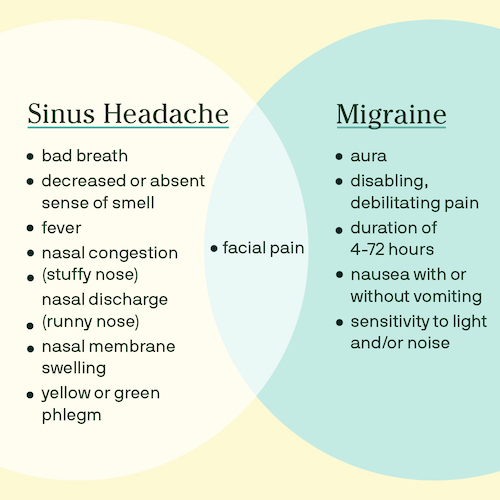
Despite what OTC sinus product makers tout, “true” sinus headaches are actually quite rare. Migraine and sinus headaches are associated with pain over the forehead and/or cheekbones. They both often are associated with swelling of the nasal membranes. That is why patients (and even doctors) may confuse the two. However, there are many differences between sinus and migraine headaches.
What’s the difference between a sinus headache and a migraine headache?
While sinus headaches are caused by a viral or bacterial infection, the cause of migraine headaches is, in large part, unknown. It involves a complex interplay between nerves, brain tissue, blood vessels, and brain chemicals. What makes it so complex is that in addition to the cause being unknown, they can be triggered by almost anything, from red wine, to bright lights, to not getting enough sleep one night (more on migraine triggers here).
While migraine pain can be noted in the cheek area and involve nasal membrane swelling like sinus headaches, they’re often associated with very different symptoms.
For example, migraine can be associated with light and/or sound sensitivity and nausea, with or without vomiting. These are only seen with sinus headaches on very rare occasions. On the flip side, migraine headaches are typically not associated with thick discolored nasal discharge or fever.
How do migraine symptoms compare to sinus headache symptoms?
Migraine symptoms can include:
- aura
- disabling, debilitating pain
- duration of 4-72 hours
- facial pain
- nausea with or without vomiting
- sensitivity to light and/or noise
Sinus headache symptoms typically include:
- bad breath
- decreased or absent sense of smell
- facial pain
- fever
- nasal congestion (stuffy nose)
- nasal discharge (runny nose)
- nasal membrane swelling
- yellow or green phlegm
How do you treat sinus headaches?
If you think you have a sinus headache, consider taking a hot shower, using a Neti Pot and/or warm compresses to loosen up the secretions. Make sure to hydrate with warm liquids like chicken soup and tea. You can try to reduce nasal membrane swelling with a short course of a decongestant and/or an over-the-counter nasal spray like fluticasone (but for no more than three days). Facial pain may improve with acetaminophen or an NSAID. If the symptoms persist for more than 7-10 days, you should see your doctor as a prescription for an antibiotic may be needed.
How do you treat migraine headaches?
If you'd like to learn more about migraine treatments and getting advice for your migraine attacks, speak to a licensed Cove doctor today about your migraine history and get a personalized treatment plan.
The information provided in this article is not a substitute for professional medical advice, diagnosis, or treatment. You should not rely upon the content provided in this article for specific medical advice. If you have any questions or concerns, please talk to your doctor.
Photo by Ben White on Unsplash.


