Like many people, you probably have a favorite season. Maybe you love snow, or the feeling of nature coming back to life in early spring, or pumpkin spice season (no judgment here).
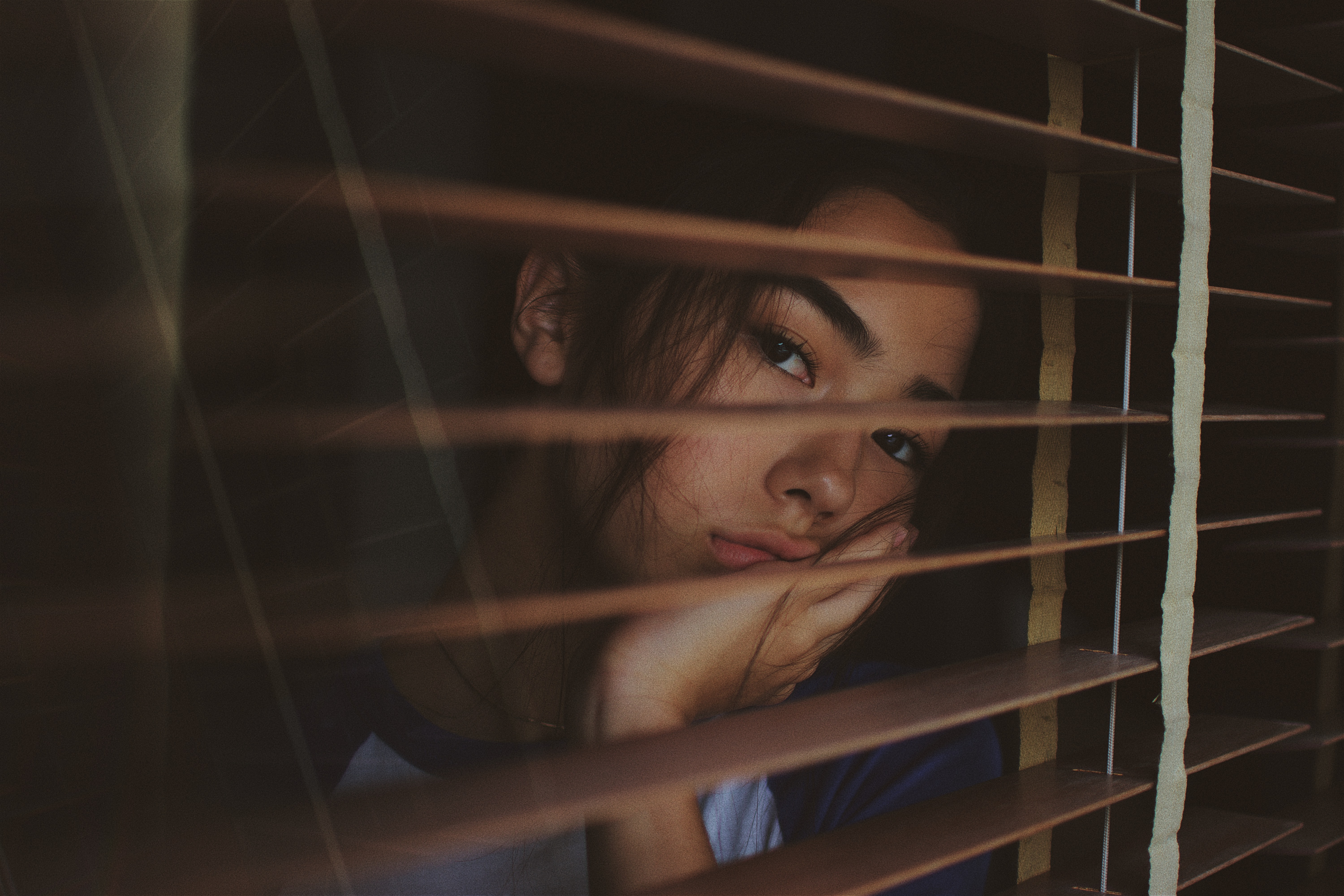
On the other hand, some seasons might get you down. Lots of people feel blue when the days start getting shorter, for instance. You might feel more tired than usual and have trouble motivating yourself to do things you normally enjoy—and before long, all you want to do is wrap yourself in blankets and enjoy your favorite comfort foods.
You may know there’s a name for this: Seasonal Affective Disorder (SAD) or seasonal depression. But did you know there’s a link between SAD and migraine?
What is Seasonal Affective Disorder, exactly?
The first thing to know is that feeling lousy in the winter isn’t just in your head—it’s a real medical condition. According to the American Psychiatric Association (APA), Seasonal Affective Disorder is a type of depression. People with SAD experience depression symptoms during certain times of the year, which can include:
- changes in appetite, especially craving carbohydrates more than usual
- decreased sex drive
- difficulty concentrating or making decisions
- fatigue and sleeping too much
- feeling sad, worthless, or guilty
- irritability and anxiety
- losing interest in activities you normally enjoy
- physical problems like headaches
- thoughts of death or suicide*
Most often, the symptoms occur in fall and winter when there’s less sunlight; January and February tend to feel the worst (in the Northern Hemisphere, that is). Experts think the shorter days actually trigger a chemical change in your brain that causes your symptoms. However, some people experience SAD the other way around and find their symptoms show up in the summer.
Now, you didn’t see migraine on that list of symptoms above, but we did mention headaches. So you may be wondering…
Can SAD cause migraine headaches?
Directly, no. Those headaches that can sometimes happen with SAD aren’t specifically migraine attacks.
On the other hand, some of the symptoms of SAD can certainly trigger attacks. Most notably, oversleeping. (Unfair, we know.) In addition, diet and exercise can play a big part, so if SAD is changing your eating or workout habits, that could also be to blame for an uptick in headaches.
What’s more of a drag is the link between migraine and depression in general. While doctors aren’t entirely sure what causes migraine or depression, let alone how they’re connected, we do know that people with migraine are over 2.5 times more likely to suffer from depression. As if dealing with just one wasn’t bad enough, it turns out that having either migraine or depression increases your chances of experiencing the other.
So why are my migraine headaches worse during certain times of the year? Can migraine be seasonal too?
While “seasonal migraine” isn’t an official diagnosis, plenty of migraine sufferers do report experiencing more attacks during particular times of the year. If seasonal migraine isn’t real, then what’s going on? Oftentimes, what they’re noticing are attacks triggered by seasonal weather changes, like:
- barometric pressure changes
- bright sunlight or glare
- extreme heat or cold
- high or low humidity
- high wind speed
- storms, lightning, or thunder
Even if weather alone doesn’t usually turn into an attack for you, it can make headaches more likely to happen when you also encounter your other migraine triggers. Besides weather, some other triggers that can occur seasonally include:
- changes to your sleep schedule when the nights start getting longer
- dehydration, which can be more common in the summer
- disruptions to your normal routine when you’re on vacation, including “let-down headaches” you may get when you start to relax
- seasonal allergy symptoms like coughing, sinus pressure, and sneezing
And of course, Seasonal Affective Disorder.
How do I know if my migraine attacks are related to SAD?
Track your migraine attacks. (In fact, that’s usually the answer anytime you want to know if your headaches are related to anything.)
Keeping track of your migraine and SAD symptoms will help you figure out if there’s a connection between the two. You can also include the day’s weather in your headache diary to see if there are any weather conditions that could be triggering attacks as well.
And if you’re sure there’s a seasonal element to your migraine, your next question may be…
How can I treat my seasonal migraine attacks?
There are two main ways to treat migraine attacks: managing the triggers and treating the symptoms themselves.
Avoid or prepare for seasonal triggers
Depending on your individual triggers, you might want to consider:
- getting the right treatment for your allergies
- keeping a consistent diet and sleep schedule no matter the time of year
- staying hydrated when it’s hot outside
And since some weather triggers are unavoidable, be prepared to take your acute medication if migraine does strike.
Treat your SAD symptoms
When it comes to Seasonal Affective Disorder, treatment can be a little trickier because you often see experts recommending light therapy or exposure to sunlight, which can itself be a migraine trigger. If you have both SAD and sensitivity to light, this approach may not be right for you.
Fortunately, other ways to manage depression like lifestyle changes, antidepressants, and therapy can be good treatment options as well. (Whenever it comes to your mental health, we always recommend talking to your doctor about a treatment plan.)
Keep up your normal migraine treatment routine
Otherwise, you can treat seasonal migraine attacks just like you would any other attack: Take your medication or supplements, use any alternative treatments or home remedies you like to rely on, and stay away from your other triggers as much as possible.
We know this sounds like a lot to figure out, and it can be. If you need help putting together a treatment plan that works for you, Cove has doctors who specialize in migraine available to assist. Connect with a doctor today.
*If you’re struggling with suicidal thoughts and need immediate assistance, please call 911, or contact the National Suicide Prevention Lifeline at 1-800-273-8255 or en espanol at 1-888-628-9454.
The information provided in this article is not a substitute for professional medical advice, diagnosis, or treatment. You should not rely upon the content provided in this article for specific medical advice. If you have any questions or concerns, please talk to your doctor.
Photo by Joshua Rawson-Harris on Unsplash.